Debt and Geography
Geography of Medical Debt from The Atlantic Monthly examines the prevalence of unpaid medical bills across the US state by state. This was from from a study out of the Urban Institute.
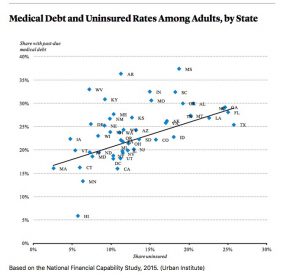
Approximately 25% of American Adults under the age of 65 had medical debt with the southern US being hit the hardest. Lowest rate of medical debt was Hawaii at 6% of adults. The highest was Mississippi at 37%. Nationally African-Americans and those between 25 to 34 years of age were most likely to have past-due doctors’ bills.
There is a high correlation between past-due medical debt and a state’s uninsured rate.
The study lays out various reasons for the geography of medical debt.
- High deductibles
- Co-Pays
- Services not covered
- Insufficient savings
- Balance Billing
“This study highlights a common criticism of Obamacare—and the overall health-care system—from both the right and left: People might be able to afford an insurance card, but they might still end up slammed with bills they can’t pay or don’t understand”
This issue of medical debt is a lingering issue that has as much harm for the patient and family as the illness. The current ACA replacement ideas are not addressing this issue. Health-savings account the high-deductible plans are not going to fix this issue. And tax credits are not weighted by income. Rich or poor get the same tax credit.
In the end healthcare is complex and there are no one size fits all or fixes all. It is a matter of what do we pick and choose to fix and who gets hurt. Right now with those in power it is singling out the poor to benefit the rich in matters of health.
EMR and Patient Understanding
Journal of Medical Internet Research published the following “Readability Formulas and User Perceptions of Electronic Health Records Difficulty: A Corpus Study” Jiaping Zheng, MS from the University of Massachusetts identified the objective of the study
“The objective of our study was to explore the relationship between the aforementioned readability formulas and the laypeople’s perceived difficulty on 2 genres of text: general health information and EHR notes. We also validated the formulas’ appropriateness and generalizability on predicting difficulty levels of highly complex technical documents.”
Conclusions suggested that readability formulas’ were not ideal predictors of the reading difficulty of EHR by patients. The formulas correlated with each other yet they did not predict patient readability of EHR.
Two outcomes I see here. First, creating a new readability formula will likely not happen in the near future and if does happen I am not sure we can expect it to widely used for EHR and if the record needs to be fixed for readability will it be done. In a word no. Second, I see engaging patients with a HCP to give them a short 101 on how to read or what to read on and EHR specific to the patient and their medical needs. This later idea will help overcome that gap in understanding. But more important it will be another engagement tool between the patient and the physician. And that will yield better long term outcomes for patent health.
Millennials and Healthcare What’s not to love
The group we old folks love to hate have some interesting and telling views on healthcare. The Medical Futurist looked at a Gold Sachs research report about millennials and focused on the healthcare portion.
Here are some highlights
When asked if they think they care more about their health than their parents of grandparents.
- 43% Yes
- 22% No
- 36% Equally
The entire digital health apps and sensors was a bit of a surprise.
Do you use any health apps?
- 15.7% I use regularly
- 31.2% I have some on my phone/tablet but don’t use them regularly
- 45.7% I don’t use any
- 4.4% I don’t have a device
How would you feel about using sensors as well?
- 28.9% I don’t care that much to try one
- 17.4% I’d rather give a pass on it
- 25.6% Neutral
- 16.2% I’d rather give it a try
- 11.7% I’d definitely like to have one
When asked which can be more efficient in urging someone to a healthier lifestyle they responded:
- 17.6% New health technologies
- 69.6% Society’s impact
- 12.8% Other
Social motivation is the primary driver for healthcare in this population. They seem to single out education from companies who sell products to having incentives built into medical insurance.